Summary
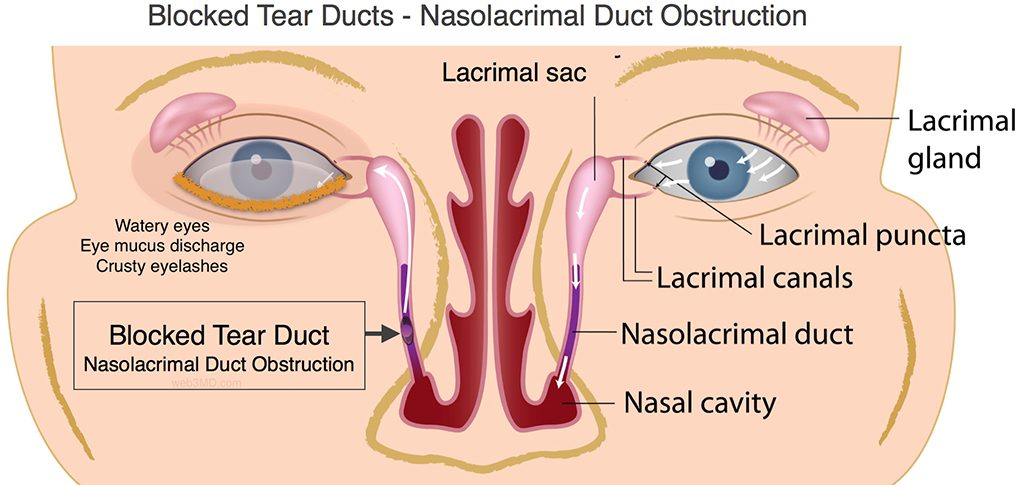
The nasolacrimal duct, also known as the tear duct, carries tears from the lacrimal sac into the nasal cavity. The nasolacrimal duct begins in the eye socket between the maxillary and lacrimal bones. Nasolacrimal duct obstruction is blockage of the nasolacrimal duct, which presents with excessive tearing. This can predispose to secondary bacterial infection of the lacrimal sac, known as dacryocystitis. Treatment is often conservative, but may also require antibiotics or invasive interventions to relieve the obstruction.
Aetiology
Causes of nasolacrimal duct obstruction:
- Congenital nasolacrimal duct obstruction: nasolacrimal duct obstruction at the valve of Hasner caused by a developmental abnormality. This is the most common cause of nasolacrimal duct obstruction.
- Acquired nasolacrimal duct obstruction:
- Age-related stenosis of the nasolacrimal duct
- Trauma due to nasal fracture or sinus surgery
- Granulomatous disease: sarcoidosis, granulomatosis with polyangiitis, tuberculosis
- Tumour: e.g. maxillary and ethmoid sinus tumours causing blockage of the duct
- Punctal stenosis due to chronic conjunctivitis and reaction to eye drops
Clinical features
Congenital nasolacrimal duct obstruction is usually seen within 3 to 12 weeks of birth. Patients present with a history of excessive tearing (epiphora), either unilaterally or bilaterally. Epiphora is also present in acquired nasolacrimal duct obstruction.
Diagnosis
Congenital nasolacrimal duct obstruction:
This is a clinical diagnosis. Probing of the duct may help identify the site of obstruction and help relieve the obstruction. Presence of ocular infection is a contraindication to probing.
Acquired nasolacrimal duct obstruction:
This is also a clinical diagnosis. Reflux when probing and irrigating the lacrimal drainage system with saline, with or without fluorescein dye, indicates stenosis of the lacrimal apparatus.
Management
Congenital lacrimal duct obstruction:
This condition usually resolves spontaneously by around 9 months of age. Before 12 months of age, management is conservative and involves lacrimal sac massage. In infants with persistent epiphora despite lacrimal sac massage, lacrimal duct probing can be used to determine the site of obstruction and relieve the obstruction. This is usually performed in infants older than 12 months of age, under general anaesthesia. Probing involves inserting a flexible metallic probe ranging from 0.7 mm to 1.10 mm in diameter through the lacrimal punctum after dilating the punctum.
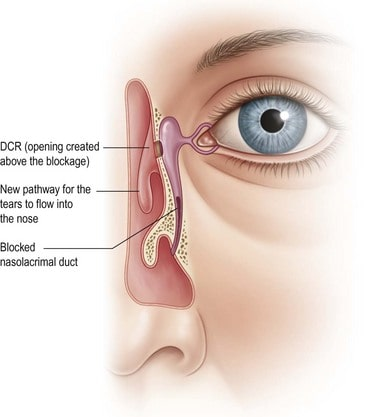
Other interventions include dilation or stenting of the obstructed nasolacrimal duct. If other measures fail, endoscopic dacryocystorhinostomy may be considered. This is where a passage is created between the lacrimal sac and the nasal cavity surgically, to provide a new pathway for tears to drain.
Acquired nasolacrimal duct obstruction:
Management of acquired nasolacrimal duct obstruction involves treating the underlying disorder. Lacrimal duct probing is used in all patients with acquired nasolacrimal duct obstruction. Endoscopic dacryocystorhinostomy may be used in refractory cases.
References
- Nasolacrimal Duct Obstruction, Congenital – EyeWiki. https://eyewiki.aao.org/Nasolacrimal_Duct_Obstruction,_Congenital. Accessed 3 Apr. 2022.
- Overview | Endoscopic Dacryocystorhinostomy | Guidance | NICE. https://www.nice.org.uk/guidance/ipg113. Accessed 3 Apr. 2022.
- Pediatric Eye Disease Investigator Group, et al. ‘Primary Treatment of Nasolacrimal Duct Obstruction with Nasolacrimal Duct Intubation in Children Younger than 4 Years of Age’. Journal of AAPOS: The Official Publication of the American Association for Pediatric Ophthalmology and Strabismus, vol. 12, no. 5, Oct. 2008, pp. 445–50. PubMed, https://doi.org/10.1016/j.jaapos.2008.03.005.
Author
Rohan Shankarghatta
Rohan is a 4th-year Medical student at KCL. He founded Doctors do Mind this past academic year focussing on the mental health aspects and pressures doctors and other healthcare professionals face in their careers. Doctors do Mind hold teaching sessions and events for students at KCL preparing them for the transition to Junior doctors by equipping them with the tools to overcome any challenges they may encounter including stress, burnout and mental health. Rohan is interested in medical education and med-tech opportunities and is always on the lookout for challenges outside the clinical space.